- The Laboratory
- Organization
- Departments
- Jobs
- Analysis book
- Contact
- News
- Publications
- Download


 As part of the LNS Annual Report 2018, we conducted a series of interviews and reports to better present the LNS through its staff and departments. This is the third interview featuring Prof. Dr. Michel Mittelbronn, neuropathologist and head of the National Center of Pathology, followed by the corresponding report. Enjoy your discovery!
As part of the LNS Annual Report 2018, we conducted a series of interviews and reports to better present the LNS through its staff and departments. This is the third interview featuring Prof. Dr. Michel Mittelbronn, neuropathologist and head of the National Center of Pathology, followed by the corresponding report. Enjoy your discovery!
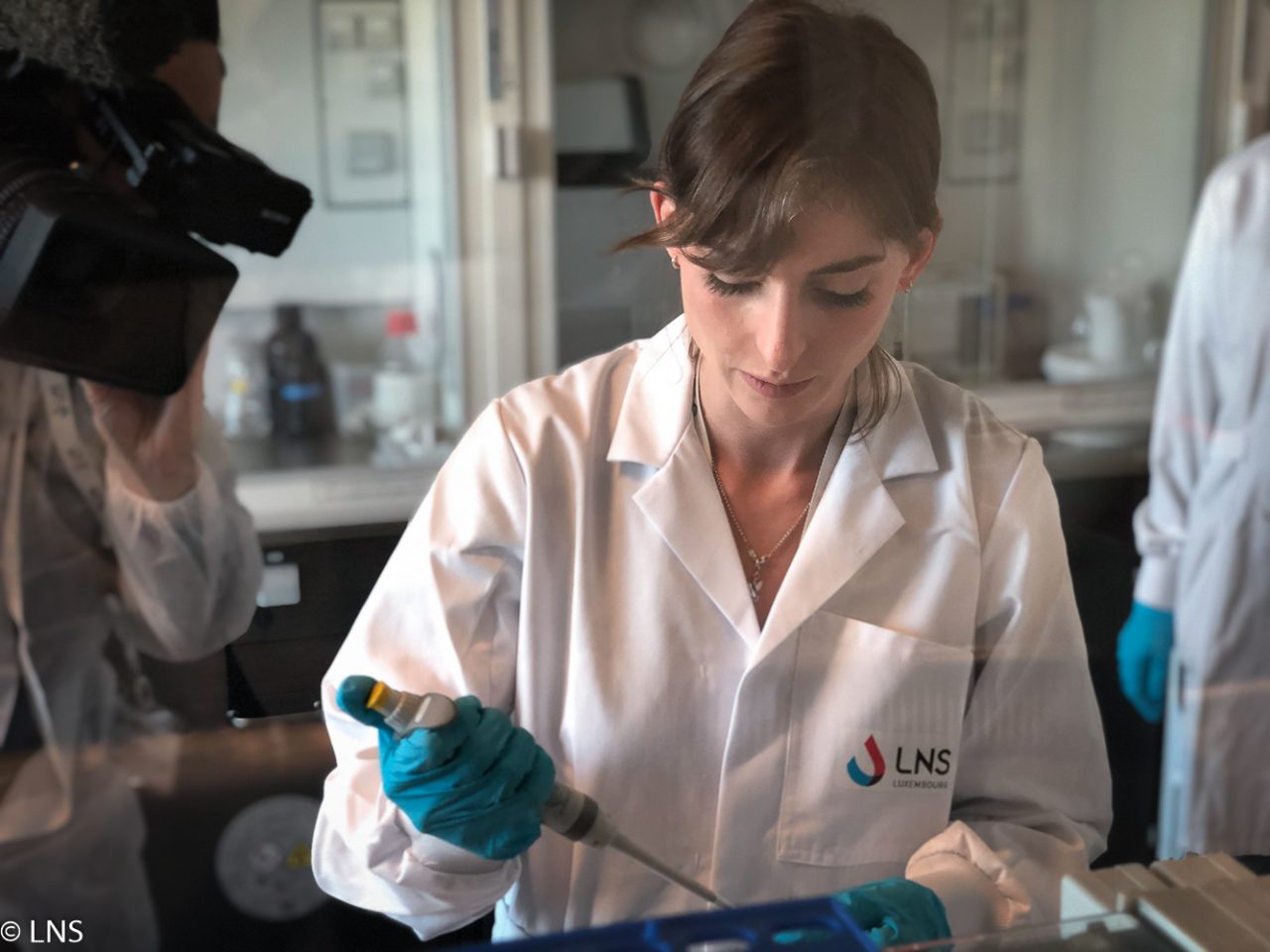
The department of anatomic and molecular pathology, now the National Center of Pathology (NCP) since 1 April 2018, is the largest department in the LNS. It is involved in the care of a large patient population, analysing more than 180’000 samples per year and is divided into two divisions: gynaecological cytology and anatomic and molecular pathology.
10 TO 15% OF IMPRECISE DIAGNOSES WITH STANDARD METHODS
The National Center of Pathology is increasingly involved in the establishment of new techniques and new molecular tests such as DNA methylation-based classification of tumours. Based on epigenetic biomarkers, this new method improves tumour diagnoses significantly. “While traditional genetics explains the way the DNA sequences are passed on from one generation to the next, epigenetics describes how genes are regulated in different cell types”, commented Prof. Dr Michel Mittelbronn, head of the NCP. “We know that a part of how epigenetics work is by adding and removing chemical tags to DNA. These tags highlight particular genes with information whether they should be switched on or off. They are called methyl groups and are used to modify one of the four chemical bases adenine (A), guanine (G), cytosine (C) and thymine (T) that make up the genetic code of our DNA. The base usually tagged with a methyl group is cytosine. When cytosine is methylated, the DNA maintains the same sequence, but the expression of methylated genes can be considerably different. Since a few years, we have discovered that DNA methylation is quite stable in different tumour entities and that many tumours have their own specific epigenetic methylation profile. By classifying tumours according to their epigenetic signature, we can classify them more accurately.”
According to Prof. Dr Michel Mittelbronn, this new tool can change a diagnosis in up to 15% of prospective cases. “With the standard methods such as the microscopic analysis, we, as neuropathologists, probably classified between 10 and 15% of all tumours in an imprecise manner. These imprecise diagnoses are not related to a lack of knowledge but might be related to multiple reasons. The tissue may be difficult to access or a large resection would be too invasive and therefore dangerous for the patient. In addition, pathologists are usually making a subjective interpretation of the microscopic image, which might be prone to subjective biases. For example, we frequently have to diagnose cases with the question if a tumour is benign or rather malignant. At first glance, some tumours appear morphologically benign and would therefore not require particular additional treatment. However, sometimes the epigenetic signature indicates a highly malignant tumour such as glioblastoma, one of the most aggressive brain cancers that has to be treated rapidly with chemotherapy and radiotherapy.”
THE POTENTIAL TO TRANSFORM TUMOUR PATHOLOGY
“You can compare the epigenetic signature of a tumour to the ID card of a person. Even if persons are disguised, we are able to recognise them by their ID number. It is the same logic with the DNA methylation-based classification. This powerful tool allows us to make more precise and more unbiased diagnoses, especially in neuropathology and probably also for soft and bone tissues tumours, and to better stratify patients according to treatment strategies.”
“To determine the DNA methylation patterns in samples, we are first applying a bisulphite treatment”, continued Prof. Dr Michel Mittelbronn. “When cytosine is methylated, the bisulphite treatment doesn’t change the methylation and leaves cytosine residues unaffected. In contrast, when cytosine is unmethylated, the bisulphite treatment converts the cytosine residues to uracil, one of the four bases in the nucleic acid of RNA. Afterwards, bisulphite converted DNA samples are amplified, fragmented and hybridised to chips that are then scanned by a laser-based, high-resolution optical imaging system. To make it simple, this array scanner, which can read hundreds of thousands of methylation sites very accurately, allows us to calculate the percentage of methylation according to the presence or absence of uracil in each patient DNA. This presence or absence of uracil is highlighted in different colours.”
“And it is just the beginning”, concluded Prof. Dr Mittelbronn. “This DNA methylation classification has the potential to fundamentally transform tumour pathology thanks to the next generation of machine-learning-based tumour classifiers.”